To better understand the complex system from varied professional perspectives—human, semiotics, clinical practice and patient—Bennett joined a team of multidisciplinary researchers and medical professionals from the University of Miami and other universities around the country to study this medical music. To start, the experts focused on the cognitive and behavioral connections between clinicians and the standardized alarm sounds. Often overwhelmed by the number of alarms and their collective noise, clinicians expressed the need to minimize alarm frequency without compromising the ability to indicate the level of urgency.
With over 20 years of professional clinical experience in acute care, Nichole Crenshaw, assistant professor of clinical at UM’s School of Nursing and Health Studies, can attest to the importance of reevaluating alarms in a simulated setting.
“Nurses are constantly working through the varied chaos of a clinical setting while monitoring alarms and communicating priorities,” said Crenshaw. “They are exposed to alarms for 12 hours a day and their input is essential to better understand how the system can be improved,” she added.
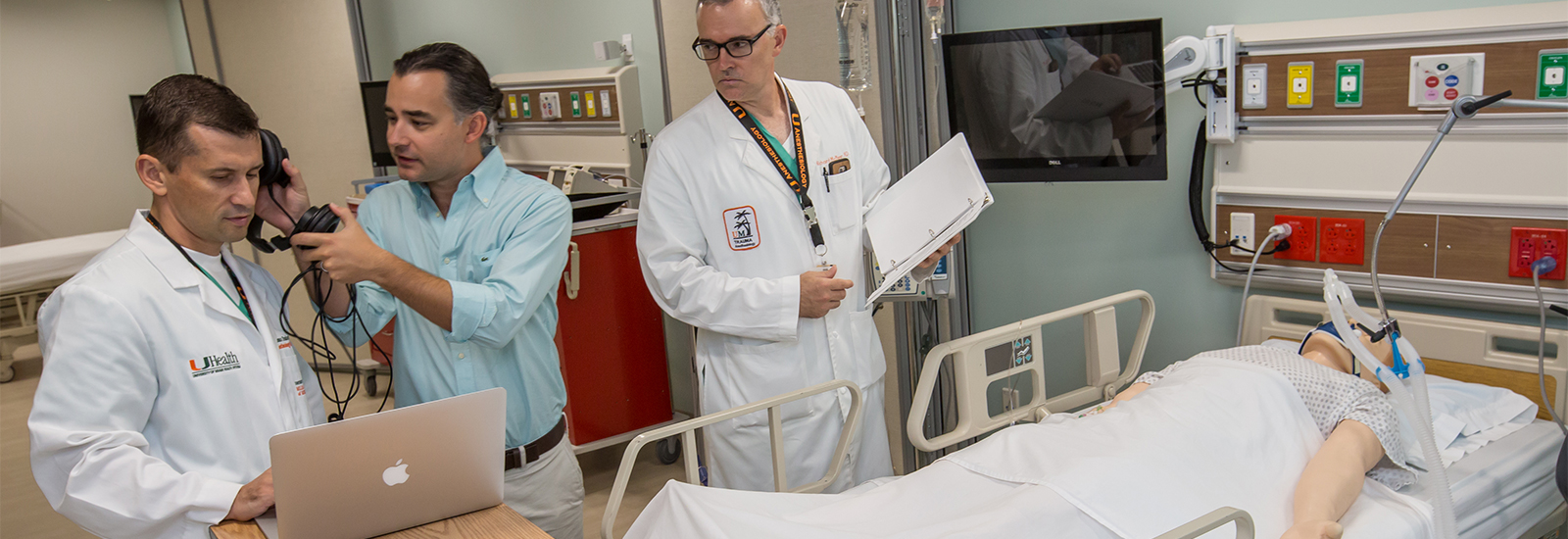
To begin testing an improved alarm system, Bennett worked closely with anesthesiologists and nurses at the UM Miller School of Medicine to introduce a system of auditory icon alarms which are meant to simulate the event it is broadcasting. The innovative medical music alarm system is being implemented in the new School of Nursing and Health Studies Simulation Hospital.
“Auditory icons are intuitive sounds, meant to mimic naturally occurring sounds,” Bennett explained. “A common example of an auditory icon is the sound of crumbled paper when using the ‘trash’ to delete a document on a computer. Within a clinical setting, the auditory icon for a ventilator alarm could mimic the sound of deep breathing, which eliminates the need for translation and allows the clinician to make a direct connection between the patient and the equipment or treatment being used.”
Throughout the study, Crenshaw and Bennett worked closely with UM doctors Richard McNeer, associate professor of anesthesiology, and Roman Dudaryk, assistant professor of clinical anesthesiology, to test and fine-tune auditory icons as replacements for the standardized alarms in a simulated operating room setting. As their research evolved, the opportunity to include additional clinical settings and students from UM’s School of Nursing and Health Studies added an enhanced perspective to the research.
“The ability to have students participate in research within a simulated setting is of extreme value to both the participants and the study,” said Crenshaw. “The study has provided students with the real-life experience of working with other clinicians and their feedback regarding auditory icons and alarms has been well received.”
Bennett’s ongoing investigation and application of auditory icons will strive to improve patient outcomes while addressing the importance and influence of sound on clinicians and patients within a clinical setting. As the research continues, nursing students and clinicians will have the opportunity to work in the new simulation hospital at the School of Nursing and Health Studies.